This blog post discusses two articles in the January 2013 issue of the medical journal Otolaryngology—Head and Neck Surgery that report outcomes for sleep apnea surgery involving removing part of the back of the tongue.
Two of the major factors that cause obstructive sleep apnea and snoring are head and neck structure (anatomy) and the muscle relaxation that occurs naturally during sleep. For an estimated 60% of all sleep apnea patients, the tongue is recognized as a major contributor, due to both of these factors. Studies have shown that weight gain can lead to the deposition of fat in the tongue itself, making the tongue physically larger. This enlargement compounds the tendency of the tongue, largely comprised of muscle, to fall backwards during sleep and block breathing.
A number of tongue-directed procedures have been developed to reduce the size of the tongue and/or prevent it from falling backwards. Many otolaryngologists are less familiar with these procedures because the techniques are relatively new and because the procedures are more difficult. As a result, I lecture frequently about how to perform them as well as how to choose the best procedure for an individual patient. Studies have shown that combining these tongue region procedures with palate procedures achieves better results than palate procedures alone. But all tongue procedures are not equal. Some tongue-directed procedures are more involved, such as the family of procedures that remove part of the back of the tongue (under the umbrella term of “midline glossectomy”) and the tonsil on the back of the tongue (lingual tonsillectomy).
Evolving Techniques and Decision Making for Midline Glossectomy
When the midline glossectomy technique was first described, surgeons used standard carbon dioxide lasers or electrocautery to perform the procedure, but this resulted in substantial swelling, pain, and risks. Newer technologies have reduced the risks, but a major question for surgeons is who can benefit from the less-involved procedures such as tongue radiofrequency or genioglossus advancement and who needs a procedure like midline glossectomy. Studies have shown consistently that heavier patients, perhaps due to their enlarged tongues, do not do as well with the less-involved approaches and may need to consider a procedure like midline glossectomy. Specifically, those with a body mass index above 32 kg/m2 (you can calculate your own body mass index using the National Institutes of Health website) generally have poor outcomes with the less-aggressive approaches. With the obesity pandemic facing the world, more patients with obstructive sleep apnea are falling into this range, leading to a greater interest in the techniques and outcomes for midline glossectomy.
The New Studies of Partial Glossectomy as a Sleep Apnea Surgery
Dr. Indunil Gunawardena and other colleagues of Dr. Sam Robinson from Flinders Private Hospital in Adelaide, Australia, reported outcomes of the combination of palate surgery and submucosal lingualplasty. Sam passed away far too young in October 2010 but was a widely-respected, innovative sleep apnea surgeon who developed the submucosal lingualplasty technique (illustrations below). This procedure involves physical removal of a portion of the tongue in the central area between the major blood vessels and nerves of the tongue, followed by additional removal of tissue towards the sides of the tongue but above those same blood vessels and nerves. Among midline glossectomy techniques, submucosal lingualplasty enables more tissue removal and also enables the surgeon to see any bleeding during surgery directly. Although this is more time-consuming and performed by few surgeons, it may be well-suited to those tongues that are particularly large. I was fortunate to discuss the procedure and learn so much from Sam, benefitting from his answers to my many questions about the procedure. While the procedure has numerous challenges, the importance of this paper is to show that the results were excellent. Three-quarters (74%, 20/27) achieve a major improvement in their breathing patterns, based on at least 50% reduction in the apnea-hypopnea index to a level below 15 events/hour (no or mild sleep apnea). The average apnea-hypopnea index decreased from 44 to 12 events/hour, and the improvement was even more dramatic for those with moderate-to-severe sleep apnea. In addition, there were improvements in sleepiness and snoring and relatively few complications.

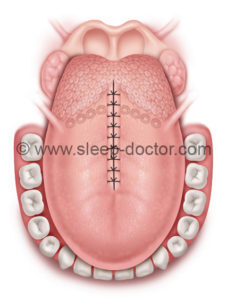
Tongue, showing location of blood vessels in blue and central area for removal during initial stages of submucosal lingualplasty procedure.
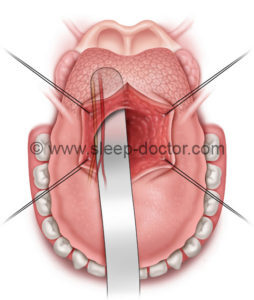
Removal of additional tissue from lateral aspect of tongue during submucosal lingualplasty.
Tongue at conclusion of submucosal lingualplasty.
Dr. Gerald Suh of St. Johns-Riverside Hospital and Mt. Sinai Medical Center in New York utilized a midline glossectomy technique that started with a lingual tonsillectomy that is extended into the central portion of the tongue base, again staying away from the major blood vessels and nerves. After combined palate surgery and midline glossectomy, there was also a major improvement in breathing patterns (average apnea-hypopnea index decreased from 52 to 18 events/hour), with 56% (28/50) achieving major reductions to have no sleep apnea or only mild sleep apnea following surgery. Gerry produced a detailed analysis, taking the critical step to examine factors that were associated with better outcomes: markedly enlarged lingual tonsils, relative tongue size, and the severity of sleep apnea. These all make sense. The larger the lingual tonsils, the more space that is created for breathing when they are removed. Because there are limitations on the extent of tongue tissue removal, those with the largest tongues did not do as well (29% vs. 76% success). Finally, when you are starting out with an apnea-hypopnea index above 60 events/hour (well in the severe sleep apnea range), it can be more difficult to end up with no sleep apnea or mild sleep apnea after surgery.
The Bottom Line: Tailor Your Treatment of Sleep Apnea to the Patient
Tongue resection procedures, under the umbrella term of midline glossectomy, are often necessary for those with enlarged tongues and/or lingual tonsils. Surgeons must understand the factors that play a role in sleep apnea in individual patients and how specific procedures work to restore normal breathing. Even among the midline glossectomy techniques, the more-aggressive options (like submucosal lingualplasty) may be needed to address the most-challenging patients, but less-aggressive options have an important role. At the risk of being redundant, these two publications reinforce the principles of having a wide array of procedures available to treat the diversity of patients with sleep apnea rather than treating every patient with the same procedure. The balance between risks and benefits is key. You do not need a sledgehammer to drive in a nail, and you certainly would not want to use a nail hammer to drive in a railroad spike either.



S,henn says:
I have a lingual tonsil on the right side of my tongue,sometimes very painful,our nose ear speacialist told me to try and life with it?beacause there are too many risks?is it so?thanks
Dr. Kezirian says:
There are definitely risks to consider, but if this area is the cause of substantial pain, the shorter-term pain and risks of a surgical procedure may be worth it. You should certainly discuss this with your doctor and consider obtaining a second opinion.
Joseph says:
Hi, I am tired of being tired, I am tired of my brain fog and forgetfulness, I see a substantial decrease in my cognitive thinking-decision making has been severely altered, ie staring at menus, staring at my choice of jackets or shoes have been become hard to make-and becoming harder on some days. Anyway, I am thin, 51 year old male, severe osa. CPAP was horrible, ( a pulmonologist put me on it) I couldn’t do it for a number of reasons, then referred to an ENT (old name I know, but the new term is annoying), he said my nasal cavities are so screwed up that having another deviated septum surgery (I had one done 20 years ago) would not alleviate the osa, dismayed, I was then sent to a dentist for a mandibular device, to shove my lower jaw forward, I had the mold done, and experienced severe saliva, and I couldn’t swallow it and choked (you can’t swallow with that device, not to mention I have a lot of mucus draining, allergies. I freaked out pulled the thing out of my mouth. I will not use that again. I was told that my tongue is too big and my soft palate is the root of my troubles and got a second opinion from a Park Avenue doctor. I was told that surgery isn’t always effective and that it is very invasive and painful I wouldn’t be able to eat or talk for a week or two. I was told by the snotty ent, that I had better get used to the CPAP or I would need a tracheotomy and I better quit smoking, (which I do want to do, but haven’t yet). I exercise and eat pretty good, I am a type 1 diabetic on a pump, I have had bad post of reactions to anesthesia. I don’t know who to believe anymore. There’s so much information on the web, from $19 mouth pieces to all different surgeries, custom mandiblar devices like mine and different types of those, mine cost $2,700. (useless) CPAP cost me 60 a month for 2 years (now I own this worthless device). I am at a loss of what to do. any straight advice from you would be welcome. I am going to an ENT at Mt. Sinai hospital tomorrow regarding a TORS surgery consult. then I read about a Medtronic made splint for the palate (I still have the tongue issue). I am confused.
Dr. Kezirian says:
Unfortunately, your experience is not so unusual, in that people often end seeing a number of people and trying several treatment options. Most physicians and dentists just have one option that they offer to everyone they see. If you are seeing Dr. Ofer Jacobowitz at Mt. Sinai, I know him well. He is excellent and is familiar with a wide range of procedures and treatments. He can work with you to sort out the best approach for you.
B Bass says:
I am a thin 44 year old male with a very large tongue causing severe osa. I am also at a loss. Nothing works. Do you know any Doctors specializing in these procedures in Oregon?
Dr. Kezirian says:
I would consider going to Seattle to see Dr. Ed Weaver at the University of Washington. There are undoubtedly people in Oregon who would be able to treat you, but I know Ed very well. He will do a great job of explaining your options.
Brandon says:
Dr. Kezirian,
Before doing a lingual tonsillectomy do you order a soft tissue MRI of the neck? If so, how big do the lingual tonsils have to be in order for you to consider a patient a good candidate for this procedure?
Dr. Kezirian says:
There is no absolute answer. I am performing MRIs in many patients being considered for lingual tonsillectomy and partial tongue base resection, but I do not have a specific number that I use to gauge whether someone would be a candidate. It depends more on the entire picture and whether I think that a tissue resection would be likely to achieve our desired outcome without excessive risks.
David says:
Hi,
I’ve been dealing with mild sleep apnea for about 10 years. I’m 6′ 190 and slender with a gut I’m working on. lol I’ve long had what I consider a large tongue, with it spilling over all sides of my tongue when relaxed. Also very muscular and thick at the back. My sleep apnea doctors have been helpful, but I didn’t tolerate CPAP well and the oral appliance has pulled my lower jaw too far forward and I now only occlude on my front teeth. This has caused one to become very loose as it bears the brunt of contact. Not occluding on any rear teeth makes chewing a steak a challenge. I had a severely deviated septum fixed about 5 years ago and it helped somewhat. Doctor told me I had an elongated pallet. I’m in Richmond VA. Thanks for any advice.
Dr. Kezirian says:
It sounds like the oral appliance is creating issues with your teeth. A standard recommendation would be to stop using the oral appliance. Since you did not tolerate CPAP well, you should consider seeing a surgeon experienced with sleep apnea surgery. You can certainly come to see me, but you can also find members of the International Surgical Sleep Society who have demonstrated a clear interest in the field. Please let me know if there is anything else I can do.
Dell says:
Hello Dr,
I’ve been diagnosed with severe sleep apnea and I have been using the CPAP for a about 2 years now. When I use it, it works well, I get a good nights sleep and my wife doesn’t wake me up 5 times a night. When I don’t use it, it affects my sleep and I have less energy throughout the day.
Im 33 yrs old, and Ive come to the point where I just do not want use this CPAP anymore. I was totally against the surgery mainly because I’ve never had surgery and was concerned about the affects. Would you recommend I get the surgery? I would need a Modified Pharyngoplasty, SMR turbinates, and a Midline Glossectomy. I’m in Yonkers NY and my sleep doctor is Dr Gerald Suh
Dr. Kezirian says:
Dr. Suh is a good sleep surgeon that I know well. You should speak with him.
Willem Faber says:
I am 48 yrs old, 1.9 and 90 kg. I have sleep apnea and not overweight, My tongue is thick or large at the back of my throat according to the doctor. I am using a Rested AirSense10 to prevent the apnea. I run 5 km at least 3 times a week and are in a good fitness state. After using this machine for 3 months I still wake up after a few hours sleep when the air is forced out of my mouth because of my tongue’s obstruction. .This usually happens in the early morning hours. My nose is also thin and it causes me to breath through my mouth when even just having a bit of flew.
At this stage I am worried that this machine might in the long run make my diafragma lazy and eventually have a effect on my health when getting old.( By not be able to sleep without it when old) Can you please advise me on the surgery – and if it is a better solution.
Regards
Willem Faber
Dr. Kezirian says:
To the best of our knowledge, CPAP does not cause any problems like weakening the diaphragm. In general, if you are able to wear CPAP and sleep comfortably with it, you should stick with it. Surgery can be an excellent option, but it is really for people that are not doing well with CPAP (or other forms of positive airway pressure therapy). There are different ways to treat mouth opening that can be problematic for CPAP because of the air leak, and you can discuss this with your sleep physician.
Angela F Copeland says:
I snore very bad!! It makes my companion angry!!! I ‘m overweight and i went to the doctor for sleep apeana. I don’t want the machine!! I also have a thick or large tongue.Should i have surgery to stop it???
Dr. Kezirian says:
You should see a sleep surgeon and discuss the full range of options with you. They will evaluate you and discuss whether surgery is a good approach.
Zoltan Forray says:
Hello. I found this site while searching for alternative ways to address my sleeping issues and hope you can offer some suggestions.
More than 10-years ago (currently 58-years old), I was diagnosed with mild to moderate sleep apnea. I was grossly overweight (267lbs). The sleep doctors then were of the mind set of “here’s a CPAP machine – slap this on and your problems will be cured”. Nothing could be further from the truth due to numerous issues I have with the whole CPAP process. From what I read (and heard from various nurses that deal with sleep issues), this is not uncommon.
First off, I can not tolerate air moving/rushing across my nose. I have such sensitive skin, it causes me to constantly wake up to scratch so a full-face mask is out (and so are most nasal pillow devices but more about that later).
Second, I have had sinus issues my whole life. Forcing air in my nose will cause it to close / become congested) and no, a heated/humidity feature does nothing but cause me to drown in the attempts to force moisture into a closed nose or I wake up coughing for an hour or two to get the excessive moisture out of my lungs when it does get through my nose. This has caused me to use OTC nasal spray to be able to sleep at all with the CPAP machine (don’t use it during the day – only at night to sleep).
Third, all machines I have used try to force me to breath in a manner that is counter to the way I breath – I tend to take infrequent, deep breaths. Original CPAP setting was 15 – later I got a bi/auto-pap machine and currently on 7-13.
I have lost a lot of weight (down to 218 but still want to loose 10-15lbs). I had sinus surgery to correct deviated septum and turbinate reduction (my ENT says there is still room for improvement and will probably go under the knife again) but I still can not get a good nights sleep. I am >98% compliant with machine usage but still wake up feeling bad/tired/foggy-minded/out of it and often have to fight to stay awake eventhough my latest machine says I am doing great with most nights AHI being under 3 (I use the Sleephead program which seems to give me the same results as what the doctor sees via cell-phone network now that I am using the AirSense 10 machine).
I am on my 6th sleep doctor. One doctor actually asked me to find another doctor since they got tired of me complaining that I felt horrible/general malaise and the CPAP machine wasn’t miraculously solving my sleep problem.
At one point, I went to my ENT asking to have the surgery to remove my tonsil/soft palate removed but be refused. He said that wasn’t my problem – my problem was my excessive/large tongue. My dentist confirmed the “large tongue” diagnoses. He also said I have the issue of both upper/lower jaws meeting exactly at the same point.
My dentist has tried a couple of things. One was the AVEO TSD/TRD which wasn’t very if at all successful due to my frenulum and even when I cut it to make it fit, wasn’t very effective. Next we went through the process of fitting me for a MAD (took 4-tries. At one point, I broke it by simply closing my jaw – which is very strong). Unfortunately, even after adjusting to the maximum, comfortable position, a home sleep study showed it wasn’t doing much at all.
After going through numerous masks, the only one I can tolerate is the Respironics Optilife. The only reason this one works is besides not covering my nose, it had the option of a “cradle cushion”. All masks I have tried that use “nasal pillows” feel restrictive and don’t allow me to draw in the volume of air I am comfortable with. Now, the Optilife is being discontinued and so far the two alternatives I have tried did not work out.
I recently when through another sleep study – this time using the ASV option. It was a complete disaster. The process kept attempting to push air at such a high pressure, it would blow the mask off my nose. I don’t think I slept 2-hours and even then the technician said I almost never reached REM much less deep sleep (three weeks since the study was done and still waiting to talk to the doctor who I think is avoiding me since he doesn’t have any answers/suggestions on how to proceed next). The tech even suggested I look into getting some kind of medical sleeping aid/drug. I have tried melatonin with little success. Some times sleep aids make me feel worse.
I am at my wits end with this whole process and it is effecting my health/mental well being. I have stopped traveling. I have withdrawn from most activities requiring commitment/regularity since I never know how I will feel each morning or if I will collapse by the afternoon struggling to stay awake. Sleep is my enemy. I don’t wake up “feeling good” – I face each day waiting to see “how bad I feel” – some days are worse than others. Some days I can make it all day and even get out and walk 5-miles. Other days I can barely make it out the door. Yet the machine says I am doing great (i.e. AHI <=4 is considered treated).
So, I am looking at any and all alternatives/suggestions/etc.
Dr. Kezirian says:
It sounds like you are asking for some medical advice, so you should e-mail me at the Contact Dr. Kezirian page of my website. Basically, you are not alone in having major challenges with positive airway pressure. Some people, in spite of wearing it all night, never really get comfortable enough with it to sleep soundly. It would be worth considering surgical treatments, as there are some that address a large tongue. If you have lost substantial weight, it has almost certainly made your tongue smaller and less of an issue. Again, please do go ahead and contact me directly by e-mail.
Zoltan Forray says:
I apologize since it has been a while since I posted my question and your response. To update. After another sleep study using a different method, the lab/technician suggested (and the doctor agreed) to try some benzo’s to help me sleep. After trying the two most common (clonazapam and lorazapam) and having either too much of a hang-over or little to no effect, the sleep doctor abandoned me (I left 4-messages and he never returned my calls). I started my own “drug-cocktail” mix with 5mg doses of Melatonin and half a 5mg Diazapam (from an 3-year old prescription I never used up). This mix seemed to keep me asleep for 4+ hours before my nocturia trip to the bathroom and then I would return to sleep. My machine says many of my daily AHI are in the <1 daily range – often as low as .2
Since things are still amiss with my blood pressure and my sleep is still not improving enough plus many periods of waking up with the shakes/jitters, my BP doctor pointed me to a local otolaryngologist.
Office exam results were "Tonsils 1+, Friedman stage III, normal AP velopharyngeal airway caliber, Class I occlusion, Normal hyoid position, Scope showing V-shaped epiglottis, minimal lingual tonsillar tissue, mostly lateral oropharyngeal collapse on Mueller"
A DISE was scheduled. The results of the DISE:
Velum: Complete anterior-posterior collapse. No CCC.
Oropharynx: No collapse
Tongue Base: Complete collapse, 3+ lingual tonsil tissue
Epiglottis: Complete collapse, independant of tongue base, V-Shaped with lateral and anterior-posterior collapse
Interval History: I reviewed the DISE findings. Based on this I recommended a first stage of epiglottoplasty and tongue base reduction.
So, I am trying to schedule this procedure since I don't see any other way out of this conundrum and as I have said, my sleep is killing me – not refreshing me.
Dr. Kezirian says:
Thank you for your comment. I do not provide medical advice here on the blog, but you can contact me directly with questions.
Jeanne says:
I am a 59 yr woman with a long uvula vibrating on my tongue. I am constantly trying to swallow it. I also have large turbinates. I have lived this way my entire life, exhausted, never waking rested, falling asleep watching tv or reading.
I have been on CPAP for 3+ yrs, a mouth device to pull my low jaw forward for 1 yr and I wear a nasal strip across my nose every night. If I don’t wear the cpap I wake up with a headache and very groggy.
Please refer me to a couple of excellent surgeons in Richmond, VA and what do you think I can do to get my life back. I weigh 148 pounds at 5′ 2″.
Dr. Kezirian says:
I am sorry, but I do not know sleep surgeons in Richmond, Virginia.
Sharon Garcia says:
I am 1 48 year old female. i wake up in the middle of the night gasping for air. not so.much as I used to but ai wake up exhausted. i wemt to a sleep center and they said it was negative, but could not explain why I wake up gasping to breathe. I recwntly went to a new dentist wjo told me my tongue is very large and asked me if i snore and do i gasp for air. i was surprised that question coming feom a dentist. he said my tongue and my teeth indicated that i move my jaw forward to move my tongue during sleep. i was at my old dentist for 15 years and he never mentioned it. my new dentist referred me to a specialist in jaw and sleep apnea and that they offer take home tests. can you live with sleep apnea if you have a large tongue? i am slightly overweight havimg a bmi of 28. i recently loat 34 pounda but have gained back 15. m I don’t ever remember my tongue being big. I was very thin weighing about 130 at 5 4 and 3/4 when I was younger I weigh 180 now does weight gain also cause you to have weight gain in the tongue? Would surgery be the best thing for someone who has an enlarged tongue rather than having sleep apnea due to other reasons
Dr. Kezirian says:
A large tongue does not guarantee someone would have sleep apnea, but it can be a reason for it. The studies are not entirely clear, but it does seem that weight loss can result in a loss of fat in the tongue, just as weight gain can cause an increase in tongue fat. If you have sleep apnea and an enlarged tongue, you would still start with CPAP. Surgery can be an option if you do not do well with CPAP.
Jill says:
I am 66 years old and have been 120 lbs. my whole life. I have full upper dentures for about 12 years now. I have had two sleep studies and I have sleep apnea. I go to the VA clinic here in Orlando, Fla. I have tried many cpap machines with no luck. The ENT says my tongue has enlarged due possibly to the Removable of my original teeth. I am exhausted and scared of what the alternatives may be. They used the word tracheostomy and I left feeling quite confused. The VA told me they would refer me to a. Specialist on the outside. Do you know of anyone in this area and do you think this is a good idea? Thank you.
Dr. Kezirian says:
You can see Scott Magnuson at Florida ENT Surgical Specialists.
Greg says:
Is there a doctor you would recommend in Michigan? I have been to several ENTs over the years but none that offer the more aggressive midline glossectomy. Most have steered me towards hyoid suspension or the inspire device. My preference would be to treat the obstruction directly through younger base resection in lieu of other alternatives.
Dr. Kezirian says:
Please contact me directly via e-mail.
jan says:
I am a 63 y.0 female who is not tolerating CPAP machine, severe fatigue and feel my tongue is consuming my mouth.
Do you know of a colleague at Washington Hospital Center in DC that could provide me a consult?
Thank you
Dr. Kezirian says:
I would recommend reaching out to them. I do not know someone specific there myself.
Stefani Hilley says:
I am a 59 year old female with sleep apnea for as long as I can remember. I also have macroglossia so bad that my tongue always hurts from the bites on the rear sides. I also have had sinus issues my whole life and have had numerous procedures to help me breath. None last long and I am always congested and so clogged there is no air movement. I have tried crap and bipap but am noncompliance as I awake gasping for air. I often sleep with my mouth open. Argh. I have tried the dental appliance but both discs in my jaw are dislocated and this eventually caused Severe tmj. I have had several tongue reduction treatments using a laser to burn the base of my tongue and thus the scar tissue will shrink my tongue. Needless to say this did not help. I hope you can offer some suggestions and or recommend someone in GA or close. Thank you for listening.
Dr. Kezirian says:
Please e-mail me directly, and we can discuss specifics of your situation.
Sidra Starkovich says:
Can you refer me to a sleep doctor who is familiar with this treatment in Minnesota? Thank you.
Dr. Kezirian says:
Please e-mail me directly, and we can discuss specifics of your situation.
Joe G says:
37yr old male. Was highly active, skinny yet fit side sleeper.
4 years ago, noticed bursitis style pain. Pain persisted/increased despite therapy and shots. Activity decreased significantly as pain became deeper. Doctors said I had FAI and needed orthoscopic surgery. Surgery was a success.
8 months into recovery, despite therapy and shots again, same pain returns (24/7 intense bursitis style pain and deep hip pain). It’s been 2.5 years now since my surgery and I am back to square one. I have become out of shape. 5’11 lean 155lbs before, now 190lbs.
Doctors say my hip never gets rest. I sleep on my side subconsciously with no control. Even bought a recliner and wake up in it on my side. Found out I had tongue apnea.
Two questions:
1) I don’t have much of a jaw. (Not freakishly absent, but slightly noticeable) An ENT suggested jaw surgery. Which would be the ideal solution? The tongue or jaw surgery?
2) Any recommendations in Utah? I live in Salt Lake City and have already bounced around many doctors.
Any input, even small would be beyond appreciated. I would do anything to end this cycle of no sleep and chronic pain. It has been eroding my personal and professional life. Doing everything I can in other areas to stay strong and fight the good fight.
Dr. Kezirian says:
Please feel free to e-mail me directly for advice related to your specific medical situation.
Rena Frum says:
Hello Dr,
Thank you for reading my email.
I have an 11 year old son. He had his tonsils out at age 3. They were very large and he had apnea. It seemed to recessive but over the years get worse again.
He had a sleep study last month and it said he stopped breathing an average of 22 times per hour.
He looks tired. He acts tired.
The new ENT I went with referred us to a pediatric ENT. Dr Prasad Thottam in West Bloomfield, MI.
He did a scope and decided very quickly that he had large lingual tonsils that were voicing his airway. He suggested cpap or surgery.
Since my son is only 11 I prefer fixing the problem with surgery instead of resorting to a machine.
Before we have him get the lingual tonsils out, I just want to know that I’m doing the right thing.
Our old ENT Dr Leider of Farmington Hills, MI seemed great but here I am again putting my son’s life in the hands of a stranger.
I read that many times, large lingual tonsils are the result of getting pairings tonsils out. So now I feel sick thinking about it. If he gets his lingual tonsils out, will his tubal or pharyngeal tonsils start enlarging? Where does it end? What are the odds of this being all he needs?
And what are the odds of a kid getting their tonsils out causing ligual tonsils to enlarge? Is it super common? Because my other son needs his tonsils out due to apnea. I don’t want to fix a problem just to allow a worse problem to pop up in a few years.
And how dangerous is lingual tonsil removal? From what I’m reading it sounds much more dangerous than palatine tonsil removal.
Also, Dr. Thottam did not do any additional testing such as MRI. I read that anther child had large lingual tonsils and an MRI showed a mass. Should the Dr have ordered an MRI before rushing into surgery?
The Dr seemed great, but I need to know that I’m doing the right thing for my son.
Also, I brought up getting him an expander with an orthodontist and she felt he didn’t need really one but that if he did have apnea after testing that an expander may be a good idea for him that could help improve the situation. Dr Thottam agreed that his mouth was a bit narrow and an expander may be a good idea in addition to the surgery.
What are your thoughts on that?
My son is tall and very slightly chubby for his age. Maybe 5 pounds overweight. He takes after my husband who got a bad weight problem later in life so I’m nervous my son will struggle with weight later in life, so my thinning is that even if the expander just helps a bit, it’s doing him a favor for later in life even.
I would appreciate any feedback you’re willing to give me!!!
I actually have 3 sons and my middle son who I haven’t discussed also had a tonsillectomy. Very very very large tonsils run in my husband’s family. My husband had a UPPP in 2010 and currently uses an cpap or bipap I think.
Thank you!!!
Rena Frum
Very concerned mom
Dr. Kezirian says:
I appreciate your concern, as it can be difficult to know how to do the best thing for your children. I really do not treat children (although I do treat some adolescents). There has been no study showing that removing the palatine tonsils (what everyone calls tonsils) causes other tonsils to enlarge. I think people that develop large tonsils develop large tonsils in all tonsil tissue. That being said, these other tonsils may or may not present issues, even if they were to get larger than what they are now.
I would ask these questions to your surgeon and to anyone else. It sounds like you have been very thorough and have received advice from people who generally agree. That, I hope, is reassuring. If not, you should keep getting an opinion until you are more comfortable with a decision.
Mary Kay Doran says:
My orthopedic doctor ordered a cervical mri due to neck pain. The radiologist saw a mass in my throat, along with 3 herniated disks. Sent and seen by ENT at Cooper in NJ. He said I have an enlarged lingual tonsil. Order sleep test an it showed moderate obstructed sleep. I also have a burning tongue that is almost constant. I have no pain or issues with my throat. Could the enlarge lingual tonsil be causing the burning tongue? Thanks.
Dr. Kezirian says:
An enlarged lingual tonsil, by itself, would not likely cause burning tongue pain. The causes may be the same or similar, however.
Elinos says:
Hello Dr,
I am a 41 years old male with BMI of 24% and I was diagnosed with premature ventricular contractions in my heart back in Sep 2018. In search of the causes of this I ended up performing 2 sleep studies which both showed many episodes of OSA. Needless to say that I snore and gasp for air and wake up tired. My doctor suggested that tonsillectomy will solve my problems as both tonsils are really big. In addition my tongue is really fat that makes things worse. Dr said nothing about my tongue. My question is even if I remove my tonsils, wouldn’t my tongue still block the airway. I have not used a CPAP machine but I think it’s not something I can tolerate. Would a mouth piece something worth trying. Thank you in advance for your response.
Dr. Kezirian says:
With specific medical questions like this, please contact me at [email protected].
Sherron Bey says:
I recently had my tonsils, adenoids and tonsil tissue removed. My sleep apnea events were 89/per hour. After surgery events are 11/per hour. What a Great improvement. I now have a bitter taste in my mouth. Is this normal?
Dr. Kezirian says:
Occasionally, someone will have changes in taste (usually just a slight decrease in taste) that resolves within 3 months at most. I expect this to clear up as well. There are some taste buds in the soft palate, and one nice Chinese study showed that those who underwent soft palate surgery with cautery were more likely to have taste disturbances, although these were mostly minor things that patients did not notice. They also all cleared up within 6 months at the latest in this study. Based on this study, I no longer use standard cautery when performing soft palate surgery.
Lynn Longworth says:
Hi Dr Keziran
My Husband is 53 and has severe Sleep apnea due to an oversized tongue. He has P-PAP machine pushing 28PSI, he runs out of water about three times a night. He was just fitted with a mouth guard to see if surgery would work( jaw would be broke in six places and bone added, etc.) His other option given is a trachea. Both these options are horrific. Are there any other options for this type of problem that his providers are not aware of?
Dr. Kezirian says:
There are many procedures available, but it sounds like your husband is going to be a challenging case. If the issue is just the running out of water and having to refill it, then turning down the humidification and/or refilling it seem like decent options. Clearly a tracheotomy would help obstructive sleep apnea. Jaw surgery can also be helpful. The one thing I will add is that, if your husband is notably overweight, it is possible that he is affected by a condition called obesity-hypoventilation syndrome that is not improved with tracheotomy or jaw surgery (making CPAP the right choice). He should ask his doctor about this.
Bobby says:
Hi, Dr. Kezirian. I’m 45, BMI 31%, however, I’m stocky from weightlifting. The ENT here in coastal Mississippi says he doesn’t perform any sort of glossectomies. I have been diagnosed with a large tongue, and about 10 years ago an ENT suggested I have a prosthetic placed in my throat to prevent my tongue from falling back, and another suggested glossectomy. Now, CPAP is difficult r/t mask fitting, so do you know of any ENT’s near me that are more aggressive that I could see?
Dr. Kezirian says:
I would see Andrea Lewis at the University of Mississippi in Jackson.
Judith says:
My husband has been struggling with sleep apnea and snoring from over sized tongue. To date he has received few options for relief despite several consultations. He is 59 and in good shape. Is there a reputable doctor in the Dallas TX area you might suggest?
Dr. Kezirian says:
I would see Teresa Chan-Leveno at UT Southwestern.
Joan says:
Hello Dr. Kezirian,
My mother has been suffering with osa due to an enlarged tongue. She has tried CPAP and sleeping aids without success. She’s become more irritable and stressed due to her lack of sleep. Is there a physician you recommend in the South Florida area?
Dr. Kezirian says:
She should reach out to her treating physician and ask for a referral.
Neo says:
Hi Dr Kezirian.
I have been on CPAP for about 3 years – have tolerated the device and has kept my AHI <1 but recently it has been steadily increasing. I notice bite marks on the sides of my tongue making me wonder if bruxism or simply my oversized tongue is causing these aggravated problems.
ENT's have said my septum is slightly deviated, my lower mandible slightly recessed.
Dentists want $2k+ for custom oral appliances but I am hesitant.
I live in San Francisco and have seen Dr. Claman at UCSF. He referred me to a chronic fatigue specialist as my CPAP treatment is within acceptable thresholds. I feel low energy all the time and am convinced it's something physiological with my tongue/mouth size but don't know who I can trust.
Any advice?
Dr. Kezirian says:
I used to practice at UCSF and think Dr. Claman is outstanding. However, you can seek other opinions if you like. I would definitely see the chronic fatigue specialist, but you can see another sleep medicine physician, just in case they have other thoughts.
Philip says:
Dr K – thank you for posting this information and the Q&A.
I was diagnosed with a mild case of apnea In 2013 and opted to use the oral device. After years of use I became intolerant of the changes in jaw/bite and associated pain and moved to CPAP In 2019. This works well but I am both a global traveler for work and a backcountry camper and I cannot take the machine along. COVID shelter in place has given me a chance to consider options. I am 5’10” 180 so not significantly overweight and have a healthy lifestyle.
Having been told I have a ‘fat tongue’ by my sleep doctor and that surgery may be an option that could improve my condition I am now considering this and also the Inspire sleep apnea device. I am wondering about your thoughts on the merits of either approach. I live in Santa Cruz CA and any good practitioners you are aware of in this area are appreciated. Thanks in advance.
Dr. Kezirian says:
For specific medical questions like this, it would be better to e-mail me directly. I cannot give medical advice over the Internet, but I can address your questions generally.
Omar Hdez says:
Hello doctor, I’m currently trying to get some sleep next to my wife who I suspect has sleep apnea due to her large tongue and small jaw. She is 145 lbs and 5’6, she has a little bit of fat around her waist but by all means I would not call her fat. That being said I just discovered this website after googling “chewing/gulping sounds while sleeping and tossing and turning” and your blog came up. My wife is 27 years old and she wakes up feeling fatigued, or like she didn’t get enough sleep. She is also prone to sleep paralysis, happens two or three times a month. My question to you is, do you recommend any doctors in Fresno California that might help her out? I suspect she also has a deviated septum, she would jump off the roof onto a mattress for fun when she was a little kid. Thanks for your continued help for anyone with similar frustrations.
Dr. Kezirian says:
I do not know anyone who focuses in this area near Fresno, and in fact I see many patients from Fresno. We can start with a telemedicine visit (billed to medical insurance) if you like. Please e-mail me directly if you would like to discuss this more.
Joe says:
I am a 41year old male I have an enlarged tongue I am uncomfortable with my tongue I bite it a lot and I lisp while talking and Im snoring. Do you know any Doctors specializing in these procedures in NY?
Dr. Kezirian says:
It sounds like you should see a sleep medicine physician or sleep surgeon. If you are interested specifically in the Inspire Upper Airway Stimulation technology, you can find centers (there are many in New York) on the Inspire Medical Systems website.
Ramsin says:
Can a large tongue still be an obstruction/compromise and individuals sleep given the following other factors?
– Nasal airways clear after septoplasty etc. procedures completed
– CPAP used with nasal mask
– Chinstrap and mouth tape used in conjunction
Am still having trouble with consistency of the result of my sleep therapy, am looking into using better mouth tape to prevent leaks or procedures such as midline glossectomy or submucosal lingualplasty. Does a large tongue still obstruct airway when you are breathing through your nose at while sleeping? Will these procedures improve sleep quality for someone with the above mentioned sleep therapy?
Dr. Kezirian says:
The tongue absolutely can still be a source of airway obstruction after treatment of nasal obstruction. Chin strap and mouth tape are not going to resolve much of anything in sleep apnea. CPAP should address tongue-related obstruction if you are comfortable with it, but tongue-directed surgery may be an important cause of sleep apnea and worth treating if someone is not doing well with CPAP.