Note: our 19th Annual Advances in Diagnosis and Treatment of Sleep Apnea and Snoring course will be held on February 15-17, 2013, in Orlando, Florida. It is the largest course dedicated to snoring and obstructive sleep apnea, and it combines medical and surgical evaluation and treatment in an unique format. Please do not hesitate to contact me with any questions or if you might be interested in attending.
Soft palate surgery is the most common surgical treatment for obstructive sleep apnea in the United States and worldwide. For many years, the only sleep apnea procedure available was uvulopalatopharyngoplasty, also known as UPPP, but over the past 20 years a number of sleep apnea procedures (including other soft palate procedures) have been developed. A previous blog post and my main website include these procedures, but it can see like there are too many choices. This blog post concerns a question I am often asked by patients and colleagues: “How do you choose which palate procedure is best for a certain patient?”
This question has no easy answer. Of course, patients must always make the final decision on a procedure, but in developing my recommendation, I consider the following:
- Main cause of a specific patient’s snoring or sleep apnea (different patients have different causes)
- What the procedure does to open the breathing passage in the throat, also known as the mechanism of action
- Research studies and my own experience with a procedure
- Risks of the procedure
Snoring procedures: palate stiffening or limited tissue removal
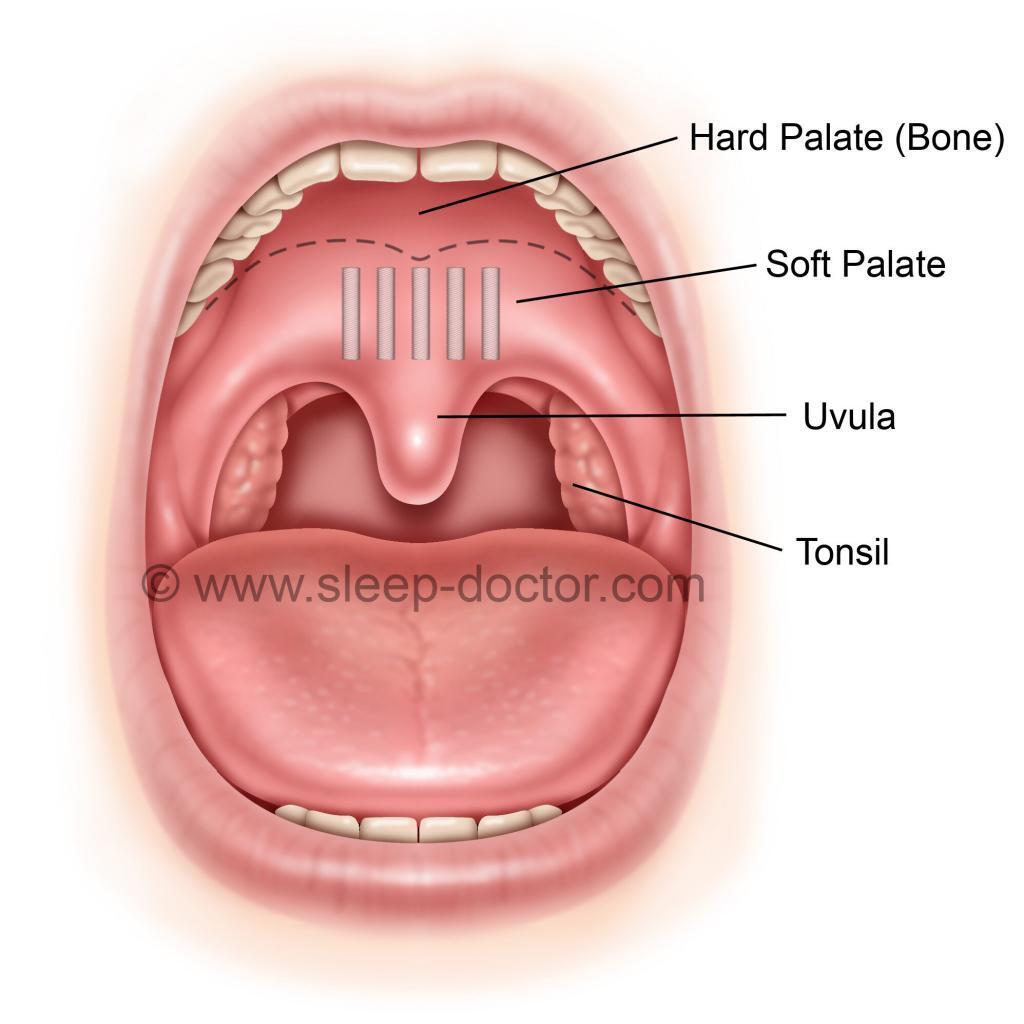
I use at least six soft palate procedures to treat snoring and obstructive sleep apnea. The Pillar Procedure (shown below) and palate radiofrequency are less-invasive approaches that can be performed in the office with relatively mild pain and lower risks than other palate procedures. They both function by stiffening the soft palate, whether through implants or by a controlled cauterization that creates scar tissue, respectively. I use these to treat patients with snoring who have soft palates that are thin or of normal thickness, although the Pillar Procedure can also be used to treat mild sleep apnea in selected patients. Many surgeons advertise themselves as experts in snoring and sleep apnea surgery and offering the Pillar Procedure as a “new” cure-all for sleep apnea. The reality is that the Pillar Procedure is both not new and not effective for most patients with sleep apnea. The best study evaluating the Pillar Procedure in sleep apnea had a carefully selected group and showed a change from 25 to 22 in the average number of times per hour with blockage of breathing (apnea-hypopnea index) after the Pillar Procedure. Although this was a statistically-significant improvement, it is not a meaningful difference for patients, which is why I only use it in selected mild cases. The reason why I perform the Pillar Procedure more often is that patients who experience substantial improvement in snoring do maintain much of this benefit, more so than for palate radiofrequency, in my experience and reported studies.
The Pillar Procedure has limited benefit in those with extra soft palate tissue bulk or a long soft palate and uvula. A long soft palate may be related to muscle or “extra” mucosa (lining of the mouth) that can exist directly behind the tonsils and function almost like a sail that flaps in the breeze, creating the snoring sound. In these cases, palate stiffening has shown limited benefit by itself, which is why I can combine some focused tissue removal, generally using cautery (more controlled and less postoperative pain than a laser, at least for me) in a procedure called uvulopalatoplasty.
Sleep apnea surgery: tissue repositioning and/or removal
For patients with obstructive sleep apnea, I use three different procedures: UPPP, expansion sphincter pharyngoplasty, and lateral pharyngoplasty (now those names are a true mouthful, pun intended). I have discussed the procedure technique as well as advantages and disadvantages for each of these on previous blog posts. Compared to UPPP, the other two procedures have demonstrated better outcomes, in scientific evaluations of the highest quality: randomized trials with patients randomly receiving one procedure or the other. Many surgeons use one procedure, which is not wrong. However, I prefer to use all three procedures, choosing among them based on the factors outlined above.
The so-called “alternative” soft palate procedures (and some others that I do not perform, at least not in their purest form) involve tonsillectomy but have less tissue removal than UPPP, instead focusing on tissue repositioning. The goal is to create a more open, stable space for breathing while also reducing potential side effects. These side effects can be related to the amount of tissue removal (less with the alternative procedures) or injury to nearby structures. Because these alternative procedures are newer and technically more challenging, fewer surgeons perform them. The techniques have also undergone revisions and modifications, and the blog posts for expansion sphincter pharyngoplasty and lateral pharyngoplasty outline the enhancements I have learned from colleagues in Singapore, Italy, and Brazil.
Choosing a procedure for sleep apnea
My goal in soft palate surgery for sleep apnea is to open the space for breathing in what I call the Palate Region. My own research has shown that many patients, after previous UPPP or palate stiffening, continue to have blockage in the Palate Region, so in my mind we can and must do better than UPPP for everyone. My opinion is that UPPP offers the most tissue removal, and I use it if I think tissue bulk is the primary issue for a patient. Expansion sphincter pharyngoplasty pulls the soft palate forward and is my preference for those with a soft palate of normal thickness or if it is slightly thin, especially in cases of posterior tonsillar pillar webbing. The one limitation is that the muscle behind the tonsils (palatopharyngeus muscle) must be sufficiently thick for the repositioning of tissue that is involved. Lateral pharyngoplasty offers the most thorough treatment of the lateral pharyngeal walls, and when I examine a patient and see marked thickening of those tissues, it will encourage to select this procedure. The reality is even more complicated, as I will combine certain aspects of the multitude of procedures that have been described in the literature in a single case. Although I discuss the type of soft palate procedure I expect to perform with every patient in advance of the procedure, I also indicate that I may reconsider the specific technique once the procedure has started and, especially, once the tonsils have been removed.
The bottom line: the same procedure is not ideal for every patient with snoring or sleep apnea
Many years ago after a lecture in another country, a surgeon asked me this same question about selecting procedures. As I was reluctant to criticize what he was doing, he mentioned that he learned how to perform UPPP in his training but did not know about these other techniques. I mentioned that the results of various research studies may not apply to his patients and that he should not feel compelled to change his practices if he was getting good results. He responded that his results were not very good but that he kept doing them because that is the only option he had to offer. What was most disturbing was that he continued without learning new techniques (his English was excellent, and he had access to medical journals) or making dedicated efforts to understand which patients had better outcomes in his own practice. Albert Einstein defined insanity as “doing the same thing over and over again and expecting different results.” Although most surgeons in the United States and around the world only learn to perform UPPP, the awareness of these other procedures is much greater than in some other countries. One of the most rewarding aspects of what I do is sharing these newer techniques during lectures or in my operating room (and this blog) and conducting studies to improve the selection of procedures. Each patient is different, requiring us to have an array of options and a method to choose among them to achieve the best outcomes in the surgical treatment of snoring and sleep apnea.




Steve says:
i have trouble swallowing because of a nasopharynx cancer I had treated. I am cancer free but my soft palete is not closing correctly to allow normal swallowing. I am on a PEG tube for nutrition and all meds. Can this be surgically corrected??
Dr. Kezirian says:
This can be treated, but it is not simple or entirely straightforward. I would recommend speaking with your doctors and asking about this. Often, you would want to wait for a period of time to ensure that you remain cancer free, as treatment (especially surgery) can make it difficult to monitor the area for possible recurrence of cancer.
kevin says:
where can i fin a doctor that does surgery in tampa area for snoring
Dr. Kezirian says:
I would see Dr. Tapan Padhya.
Donna Myers says:
I have a sleep study scheduled for obstructive sleep apnea, I also snore like a bear. I am a 70 year old female, maybe 5 to 10 lbs overweight. I live in Elon,NC, would this surgery be beneficial for me?
Dr. Kezirian says:
The first step is to have your sleep study and determine if you have obstructive sleep apnea. If you do, positive airway pressure therapy (such as CPAP) is the first-line treatment option. Surgery would be considered in you if you are not doing well with positive airway pressure therapy. If this turns out to be the case, I would recommend seeing someone who focuses in sleep apnea surgery for an evaluation to determine what might be best for you.
marlene dooley says:
Can you recommend a surgeon in Roanoke, Va area?
Dr. Kezirian says:
I do not know people in Roanoke. You might consider checking the website of the International Surgical Sleep Society (surgicalsleep.org) to see if there is anyone close to you.
Jean says:
Thank you so much for providing thorough information. Can you recommend a doctor in the Norfolk, Virginia area who is skilled in these soft palate surgeries for children?
Dr. Kezirian says:
I do not know people in Norfolk. You might consider checking the website of the International Surgical Sleep Society (surgicalsleep.org) to see if there is anyone close to you.
BRAJESH KUMAR says:
Dear Sir,
Mine is a case of a 49 yr old male 162.5 cm tall weighing around 74 kg suffering from OSA and snoring.
Epworth sleepiness scale of 7, digital skiagram of soft tissue neck lateral view result shows ‘ homogeneous soft tissue opacity in the sub mandibular region causing effacing of the oral and oropharyngeal airway’ , enlarged tongue, anterior marginal osteophytes and reduced disc spaces at C5-C6 and C6-C7.
NCCT PNS report is as follows:
Mucosal thickening is seen inbilateral maxillary sinuses. Polypoidal appearance of thickened mucosa is noted is noted in medially in left maxillary sinuses.
Mucosal thickening is also seen in bilateral ethmoidal sinuses, relatively more prominent on left side.
Mucosal thickening is also seen inferiorily in bilateral frontal sinuses.
Right sphenoidal sinus also shows Mucosal thickening . Mild Mucosal thickening is also seen in left sphenoidal sinus.
Left ostio-meatal unit is compromised by Mucosal thickening in maxillary sinus ostium region. on right side, the Ostio-meatal unit is patent.
Bilateral inferior turbinate hypertrophy is seen.
Concha bullosa is noted on both sides.
S-shaped DNS is seen..
prominence of lateral walls of nasopharynx and oropharynx on both sides . Soft palate also appears to be thick.
I have consulted three ENT surgeons, all have different line of treatment .
One suggested nothing to do except using C-PAP or BiPAP.
second advised surgery to clear the mucosal thickening of left maxillary sinus and clearing ostio-meatal unit apart form correcting for Conch bullosa.
Third surgeon advised for Ang and lateral Pharyngoplasty as wellas tongue channeling.
Please advise, the last one would be would really cure me of the sufferings.
Thanks.
Dr. Kezirian says:
You are asking for medical advice. Please send an e-mail to me directly at [email protected].
Heather McNeely says:
I am a 56 yr fit female who has suffered sleep deprivation for 33 yrs. 9 sleep labs numerous CPAP machines , plastic surgeons ,uppp surgery ,multiple RX, multiple Dr s… My GP has been trying to find surgeon or specialist for Soft Palletes in the Ottawa area since December 12th 2016. I need some help signed exhausted…
Dr. Kezirian says:
I do not give medical advice on my blog. You can contact me directly for more information about consultations on Skype or traveling for in-person evaluations.
Teresa says:
I also have sleep apnea and I think I was diagnosed of having it in 2012 I do believe and have been on my cpap ever sense I was just curious of what kind of surgery I might need and if my ear nose and throat dr. Can perform what I may have want done to see if it may help me or could it be worse that’s what I kinda to like to know before I gave anything done like that or would I have to have it done out of state I live in Pennsylvania
Dr. Kezirian says:
The short answer is that you should continue with CPAP if you are tolerating it well. A sleep surgeon can discuss potential surgical options, but it would really only make sense to pursue surgery if you are not doing well with CPAP.
Roger says:
I’m an active 38 year old male with a BMI of 27 and mild/moderate OSA and intolerant of CPAP. I’m interested in surgical options. Do you know of any sleep surgeons in the Portland, Oregon area? I could travel, if necessary, in order to be treated by someone experienced. Thanks much!
Dr. Kezirian says:
Ed Weaver at the University of Washington is excellent. Otherwise, I would be happy to see you and see many patients traveling from around the country and from other countries too. I also can do online consultations via something like Skype; since these are not billable to medical insurance, I do have to charge for them. Please let me know in advance, as we can coordinate some things to minimize the number of trips you need to make to Los Angeles.
Tahir Jaffery says:
Please note I used the cpap but not feel changing a doctor advice to operate what your opinion?
Dr. Kezirian says:
Surgery is an option for patients with sleep apnea who have not experienced benefit with CPAP, in spite of sleeping with it through the entire night, every night. There is no single right answer for everyone, but the question is why you are not feeling a change. Sometimes people are not truly sleeping comfortably while wearing the CPAP. Of course, you would also want to make sure there are not other explanations for your symptoms.
Paul says:
I’m a 50yr old male w/ OSA and very loud snoring. My most recent sleep study showed my AHI at 50. I’ve had no luck with CPAP. I live in Chicago. What area doctors/hospitals in Chicago do you recommend for exploring surgical options? My BMI is 28. (6’1″ 210lbs) Thank you.
Dr. Kezirian says:
Please contact me directly via e-mail.
Ken Murphy says:
Hello Dr. Kezirian,
I just saw Steven Park MD in NYC, a great man. I was finally diagnosed with OSA (AHI=18). He and my PCP note, I have an incredibly high palate. Park said the palate “failed to drop.”
I am not asking for personal medical advice. Generally, however, is it possible that a surgery can be performed to simply lower or bring down the entire soft palate in order to create more airway space (and less airway resistance) in the nasal cavity above? (I also have a hyponasal voice that I hate, thinking that a lower palate would allow more air to pass and my voise to resonate)
Thank you again for your help. I am impressed with your thorough mastery of your field. Dr. Park is also an incredibly erudite doctor and surgeon if you get a chance to encounter him.
Sincerely,
Ken
Dr. Kezirian says:
I know Steve Park pretty well, and I also like him very much. There are various palate surgeries. I do not usually describe palate obstruction in quite the same way, but palate procedures are designed to advance at least a portion of the soft palate and open the space for breathing.
Ken says:
Thanks very much.
Gary Puntman says:
It’s good to know that there are different procedures to choose from to help snoring and sleep apnea. I’m sure some procedures are better for some than others. I like that you said you can also combine procedures for patients to get them the best results.
Danielle Smith says:
I’m 50 and have a cpap machine. I had a tonsillectomy 2 months ago, but encountered complications. While recovering I ended up getting a TPA peritonsillar abscess/soft tissue infection. Since then my soft pallet seems to have drooped or lowered because the uvula is a lot lower (almost touching my tongue when mouth is open) and the airway seems a lot smaller. I can barely see the back of my throat now. It always feels like there is something on the back of my throat and my voice sounds a bit garglly when I talk and feels swollen after talking for a while. Is this normal for recovery? The cpap machine makes me feel like Im choking even more. The ENT said that everyone heals differently. Is this true/normal recovery?
Dr. Kezirian says:
People definitely heal differently, and I would not worry about one side of the palate looking a little different than the other. Also, the uvula does touch the tongue most of the time in all of us, so that, by itself, is not an issue. You still have some healing to do, so I would definitely allow that to occur too. That being said, you want to have an improved space for breathing and not to have other new issues.
Donna says:
Can you recommend a qualified physician in Colorado?
Dr. Kezirian says:
Please e-mail me directly through the e-mail address on my website.
shishir Majithia says:
Hi, I had just one question, how much is the cost approximately of a surgery, I live in Kenya in Africa and may require this after doing a sleep study
Dr. Kezirian says:
You have sent me an e-mail directly. I will just repeat that there are many different procedures that have different costs. Unfortunately, medical care in the United States is expensive, but with my international patients I want to discuss what procedure(s) make sense and then discuss the costs involved once we have a chance to ask the hospital for a formal price quote.
Judy says:
If surgery is not successful can it reduce the effectiveness of CPAP?
Dr. Kezirian says:
Old-fashioned soft palate surgery that removed tissue could make it so that CPAP administered through the nose would come back out of the mouth at lower pressures (compared to before surgery). In the US, surgery is reserved for those who are not tolerating CPAP, so this would not take someone who was doing well with CPAP and create problems. However, I do not perform the traditional approaches, as there are soft palate procedures based on repositioning tissue (expansion sphincter pharyngoplasty, lateral pharyngoplasty) that have shown better outcomes than the traditional approach in randomized studies. I hope this answers your question.
Shane says:
I’ve struggled with OSA since 2008. Using CPAP has never really worked well enough where I could sleep 6-8 hours per night. I’ve survived off of 4-6 hours a night wearing CPAP. I had a couple consults with two different doctors/surgeons for MMA and UPPP surgeries. MMA wouldn’t be an option for me, but UPPP is an option. Dr. Mark Wax will be performing the surgery in Portland, OR. I know the possible health concerns of having sleep apnea not treated successfully. It’s the reason why I’ve looked into other options. I’m concerned about after going through all this, will it really benefit me? Especially, since the success rate is really not high at all.
Dr. Kezirian says:
These are questions you should ask Dr. Wax. There are some patients that can do very well after sleep surgery, and results vary by patient and procedure.
If you would like a formal or limited evaluation of your case, you can e-mail me directly.
Eric VanNockay says:
Hi, Im looking for someone who does the Pillar procedure in the Orlando, Fl. area
Dr. Kezirian says:
I do not know anyone who does the Pillar Procedure there.
Trevor H says:
Hi there. 36yo male BMI around 29 here. I have a palatal prolapse causing nocturnal arousals when exhaling nasally (causing nasopharyngeal blockage). It seems I need my palate/uvula reduced/stiffened. Is there a gold standard procedure for someone with these symptoms? It seems it is not too common?
Dr. Kezirian says:
There are various approaches, including formal palate surgery and palate stiffening. This is not so unusual, so experienced sleep surgeons have seen this many times before. One challenge can be that you may be a kind of patient that tends to wake up easily, so you may really need things open in your throat to avoid the awakenings.