At the American Academy of Otolaryngology—Head and Neck Surgery Annual Meeting last week in Washington, DC, Alan Pack, MBChB, PhD delivered the Neel Distinguished Research Lecture on the topic “Towards Personalized Sleep Apnea Surgery”. This honor is reserved for those with major contributions to science in disorders of the head and neck, and Dr. Pack fits that description. A leading sleep medicine researcher from the University of Pennsylvania, Dr. Pack spoke about the need for personalized approaches to sleep apnea surgery. In discussing his own research on genetic factors important in the development of obstructive sleep apnea, he also cited some of my work related to drug-induced sleep endoscopy. Both are part of the growing body of evidence describing differences among individuals with snoring and obstructive sleep apnea that demands a movement beyond the one-size-fits-all approach that has been used for too long in sleep apnea surgery.
Here Is a Surprise: Different People Are Different
Dr. Pack highlighted research demonstrating differences among people in the factors that contribute to sleep apnea, its consequences, and the response to specific treatments. One study from Australia and Hong Kong examined obesity, a well-known factor in sleep apnea, among Caucasians and Asians (although these racial and ethnic categories are oversimplifications, the studies have tried to find groups that are fairly homogeneous). Obese (compared to non-obese) Caucasians were more likely to have obstructive sleep apnea, which was not true among Asians, in whom sleep apnea was common among those with and without obesity. However, obesity had a larger impact in worsening the severity of sleep apnea (the number of times per hour with blockage of breathing) in Asians, compared to Caucasians. This study and others suggest that factors such as facial structure likely play a more-important role in developing sleep apnea for Asians but that changes in body weight have very different effects in these two groups.
Genetics, one source of differences between individuals, has been an active area of sleep apnea research over the past few years. Dr. Pack and his team has conducted genetic research with Thorarinn Gislason, MD, PhD and others at the University of Iceland that is outlined in their review. They have identified three genes that are known to play a role in obesity, two of which also increase the risk for sleep apnea and one which surprisingly decreases the risk. The genetics of obesity involves multiple genes, and so too is the relationship with sleep apnea complex. Other genetics research in sleep apnea has shown that genetic factors may play an important role in whether someone with sleep apnea develops high blood pressure and sleepiness, one major area in which people with sleep apnea can be so different.
Surgeons need more than one hammer before looking for nails
Dr. Pack called for more rigorous sleep surgery research, incorporating all that we know about how certain patients respond better than others to certain surgical interventions. Overall, the surgical treatment of sleep apnea has demonstrated a number of important, meaningful benefits, ranging from lower risks of death or cardiovascular problems (such as high blood pressure or heart attack) to a reduction in motor vehicle crashes to improvements in sleepiness and quality of life. However, outcomes of surgical treatment for individual patients and for individual procedures have been shown to vary widely. What is clear is that no single surgical approach works for everyone. Unfortunately, those on both ends of the surgical treatment spectrum, including surgeons and non-surgeons, have what I (as well as Dr. Pack and many others) feel is a misguided perspective that is either doomed to failure or overly-aggressive.
On the one hand are those who are looking for quick fixes, using either a minor procedure called the Pillar Procedure or the surgery that has been available for 30 years (uvulopalatopharyngoplasty, or UPPP) and treating everyone with them. The most glaring example is the heavily-marketed approach adopted by some surgeons and groups that tout themselves as experts in minimally-invasive procedures for sleep apnea and offer the Pillar Procedure as the primary treatment for sleep apnea. Unfortunately, their promotion ignores the evidence that the Pillar Procedure does not work well in most patients with sleep apnea. Some websites cite one carefully-done study showing a “significant improvement” in sleep apnea that was based on a drop from 25 to 22 in the number of times per hour that there was blockage in breathing; although this is technically statistically significant, the degree of improvement is not meaningful to patients. I do perform the Pillar Procedure and can report excellent results, both in research studies and my own experience, because I limit it to two groups of patients: those with snoring who do not have sleep apnea and carefully-selected individuals with sleep apnea.
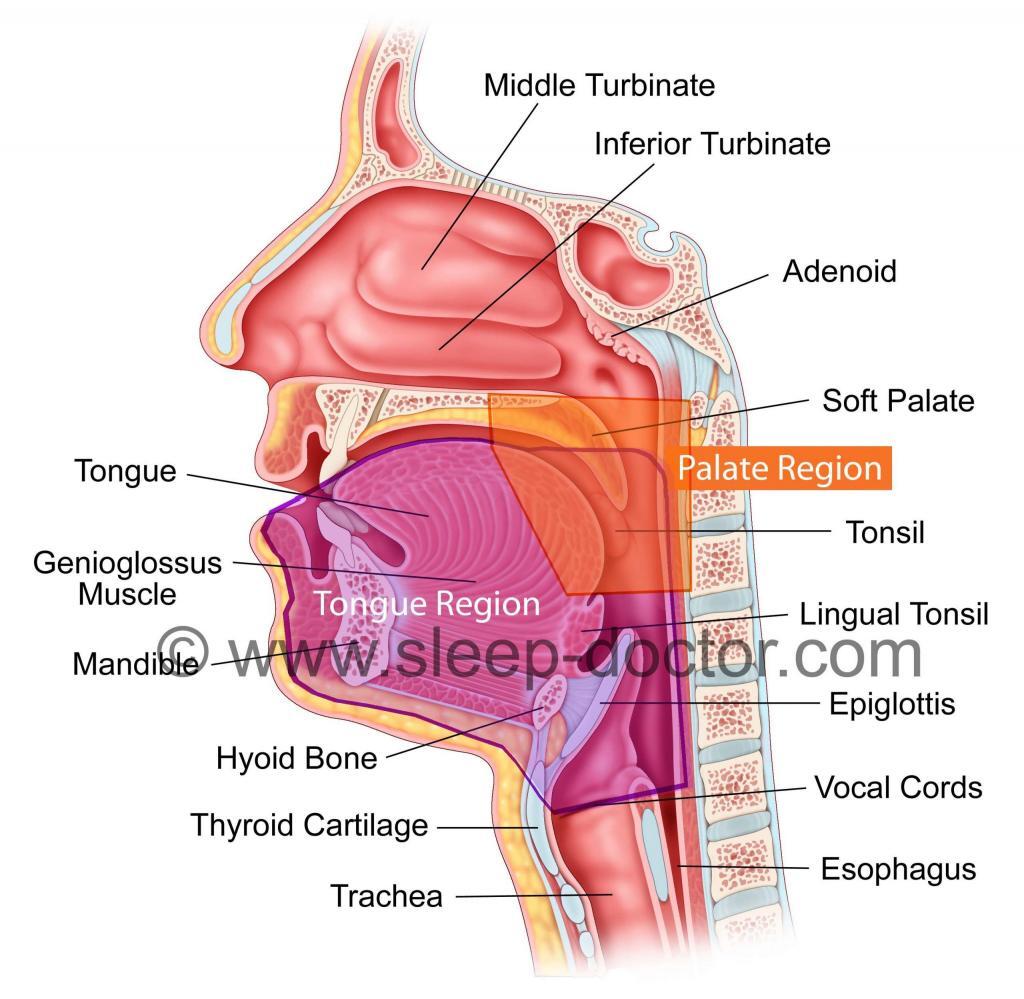
One of my previous blog postings discussed the limitations of UPPP as a stand-alone treatment for everyone with sleep apnea. There are a number of other procedures directed at what I call the Palate Region and Tongue Region (see Figure), and at the meeting I again taught a course on Tongue Region procedures and the patient characteristics that are associated with results. These patient factors are critical parts of how surgeons should make decisions regarding procedure selection and development of personalized sleep surgery treatment. There is substantial evidence supporting the benefits of personalized approaches in sleep surgery, although more research will provide even greater insight.
On the other hand are those who blindly promote maxillomandibular advancement. This is a more-involved procedure that is a great treatment option for many patients with obstructive sleep apnea. I have treated many patients with the procedure who have largely been very happy with the improvement in sleep apnea. Overall, the outcomes reported in various studies have generally been more consistent and better than for other procedures. However, this does not mean that it should be the primary (or sole) surgical option for sleep apnea. This approach is not only misguided but hazardous to patients, many of whom reject it because of its invasiveness and therefore remain untreated (as they are considering surgery because they cannot tolerate continuous positive airway pressure). Maxillomandibular advancement is not for everyone. Some people (for example, older adults) do not do as well as some studies might suggest. It is also important to consider that this is a major surgical intervention with significant, important health and surgery-related risks to consider carefully, not to mention a prolonged healing period. In my experience, I have been amazed and disturbed at how some non-surgeons promote this procedure, often more so than surgeons, while remaining relatively unaware of what the procedure entails.
Personalized treatment of sleep apnea almost certainly improves results
Personalized treatment approaches for sleep apnea are active areas of research. David White, MD and Atul Malhotra, MD, with their sleep disorders research team at Harvard Medical School and Brigham and Women’s Hospital, are leading the way in a process called phenotyping, characterizing the role of different factors (mainly nonsurgical factors) that can contribute to sleep apnea in individual patients. This has the potential to lead to personalized non-surgical treatments. From a surgical standpoint, the purpose of evaluation techniques like drug-induced sleep endoscopy is to determine, in a specific patient, the physical structures that contribute to sleep apnea. The goal of surgical evaluation is to identify those factors and develop a targeted, effective surgical treatment. Personalized approaches are used today to treat conditions ranging from high blood pressure to cancer. Every day, I rely on the large body of scientific literature, my own experience, and the preferences of my patients to make personal treatment decisions with my patients. Although there are many research studies that guide this process, further research will enhance our understanding of snoring and sleep apnea so that we can refine this personalized approach to achieve the best possible outcomes.



1 + 5 =